Digestive Disorders and Kidney Stones: What You Must Know
If you've struggled with calcium oxalate kidney stones, you may have heard digestive disorders are to blame. In this blog, I break down the truth behind conditions like inflammatory bowel disease (IBD) and chronic pancreatitis, how they influence kidney stone risk, and what you can do to take control. Spoiler: your diet plays a much bigger role than you think.
Key Takeaways
-
Digestive disorders like IBD and chronic pancreatitis are rare but often blamed.
-
The real problem is excess oxalate, not the digestive disorder itself.
-
Eliminating oxalate-rich foods greatly reduces stone risk.
-
Managing diet and hydration is key to preventing calcium oxalate kidney stones.
If you've been suffering from calcium oxalate kidney stones, your doctor may have pointed fingers at a digestive disorder. But what digestive disorders are we even talking about, and do they really cause stones?
In today's blog, I’m going to break down common digestive disorders like inflammatory bowel disease (IBD) and chronic pancreatitis. We'll explore their real relationship with kidney stones and whether you should be concerned.
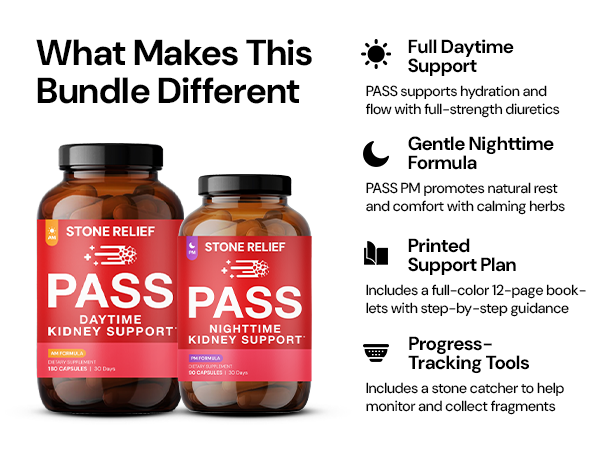
🛒 Check Price & Purchase Stone Relief Pass AM/PM Bundle on Amazon
Inflammatory Bowel Disease (IBD) and Kidney Stones
IBD is a term that covers disorders causing chronic inflammation of the gastrointestinal tract. This includes Crohn’s disease and ulcerative colitis. Many confuse IBD with IBS (Irritable Bowel Syndrome), but IBS doesn’t actually damage the GI tract.
Although doctors often blame IBD for kidney stones, it's important to know that IBD is rare. Less than 1% of the global population suffers from it. In the U.S., it affects just over 3 million people.
The cause of IBD, according to mainstream medicine, remains a mystery. But if you've been following my work, you know it ties back to diet more than anything.

IBD's Impact on Urinary Oxalate and pH
Research shows a slight increase in urinary oxalate among people with IBD. IBD patients average 42 milligrams per day, compared to 39 milligrams in non-IBD subjects. People with small bowel resectioning show even higher levels, about 57 milligrams per day.
These numbers creep close to what’s seen in primary hyperoxaluria (PH1), a rare genetic disorder. However, it's critical to understand that even though there's a rise, the data is observational and messy—not definitive.
Additionally, IBD affects urine pH. IBD patients typically show a urine pH of around 5.98, a slightly acidic environment that promotes calcium oxalate crystal formation.
The Real Issue: Oxalate, Not IBD
Despite all the finger-pointing at IBD, the real enemy here is oxalate. If you eliminate oxalate from your diet, urinary oxalate drops, and so does your stone risk. And with diet changes, many people even resolve their IBD symptoms naturally.
🛒 Check Price & Purchase Stone Relief Pass AM/PM Bundle on Amazon
The Role of Chronic Pancreatitis
Another digestive disorder often blamed for kidney stones is chronic pancreatitis. This is a persistent inflammation of the pancreas that affects both digestion (exocrine function) and hormone production (endocrine function).
Fortunately, chronic pancreatitis is rare. Less than 1% of the U.S. population is affected. Most cases are linked to alcohol consumption, especially more than two drinks per day for men and more than one drink per day for women.
How Chronic Pancreatitis Can Impact Kidney Stones
Chronic pancreatitis can indirectly increase stone risk through fat malabsorption. Here’s how:
-
Fat malabsorption causes unabsorbed bile acids and fatty acids to bind with calcium in the gut.
-
With less free calcium available, more oxalate remains unbound.
-
This leads to greater oxalate absorption into the bloodstream.
-
As a result, more oxalate shows up in the urine, increasing stone risk.
However, remember: this isn’t a problem if you don’t consume oxalate. No oxalate equals no calcium oxalate stone risk.
🛒 Check Price & Purchase Stone Relief Pass AM/PM Bundle on Amazon
Oxalate Is the True Enemy
Whether you have IBD, chronic pancreatitis, or neither, the real problem is oxalate.
As kidney stone formers, we lack the genetic or metabolic machinery to handle oxalate properly. It gets stored in our bodies—joints, glands, kidneys—causing all kinds of problems.
Plants naturally produce oxalate to deter predators. Unfortunately, our bodies are not built to process high amounts of it.
How to Minimize Your Risk
1. Eliminate Oxalates from Your Diet
The most effective step you can take is removing oxalate-rich foods. Animal foods—meat, dairy, eggs, bone broth—are naturally oxalate-free.
2. Neutralize Your Urine pH
Maintain a urine pH between 6.5 and 7.5. Test your pH daily with urine strips to ensure you don't swing too alkaline and risk calcium phosphate stones.
3. Drink a Minimum of 3 Liters of Water Daily
More hydration leads to more urine output, which helps flush out lithogenic agents like oxalate before they can crystallize.
4. Measure What You Manage
Order a 24-hour urine test about every three months to monitor your urinary oxalate levels and adjust your diet accordingly.
5. Get a Coach
Having someone who's been where you want to go makes a massive difference. Find a coach familiar with oxalate elimination to guide you through the process.
Final Thoughts
Digestive disorders like IBD and chronic pancreatitis are often unfairly blamed for kidney stones. The true root cause is oxalate.
When you take control of your diet, eliminate oxalates, and support your body with hydration and the right foods, you give yourself the best chance at true, lasting kidney stone freedom.
Ready to make a real change? Start with your plate. Your kidneys will thank you.