Understanding Calcium Oxalate Monohydrate Kidney Stones
If you've been diagnosed with calcium oxalate monohydrate kidney stones, you’re not alone. In this blog, I break down the different subtypes of these stones, what causes them, and what you need to know to prevent them for good. Getting the right information is critical to getting your life back!
Key Takeaways
-
Calcium oxalate monohydrate stones have multiple subtypes with unique causes.
-
Most types are linked to dietary oxalate intake and low hydration.
-
Some rare types are tied to genetic conditions or digestive issues.
-
Understanding your specific stone subtype is essential for prevention.
When I had my first few kidney stones, I had no idea there were different types and subtypes. It wasn’t until I got brushed off by both my urologist and general practitioner that I realized I had to dig into the research myself.
Understanding the exact type and subtype of your kidney stones is crucial if you want to prevent them from coming back. In today’s blog, I’m going to walk you through the different subtypes of calcium oxalate monohydrate kidney stones and what you need to know about each one.
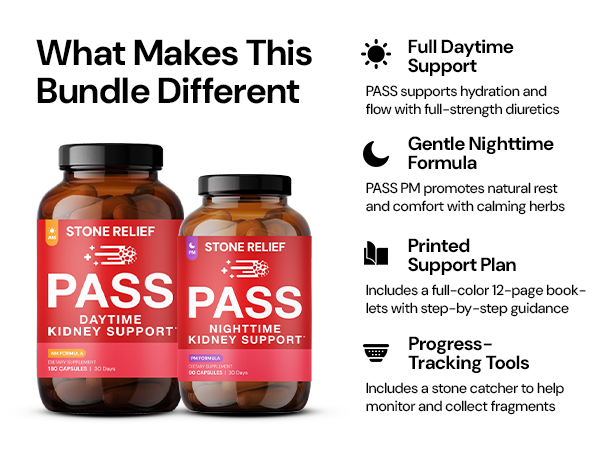
🛒 Check Price & Purchase Stone Relief Pass AM/PM Bundle on Amazon
Type 1a Calcium Oxalate Monohydrate Stones
Type 1a stones are the most common stones formed by calcium oxalate monohydrate. They are round, dark brown, and often show small surface budding. Sometimes, you’ll notice a light gray film, indicating an active stage of crystallization.
The formation of this stone is tied to secondary hyperoxaluria, meaning it’s driven by diet. Excessive oxalate intake paired with low diuresis—low urinary output, usually from poor hydration—allows calcium and oxalate to bind and form these stones.
If you passed a stone that looks like this, it’s almost certainly diet-driven. Changing your diet can completely alter your future with kidney stones.

Type 1b Calcium Oxalate Monohydrate Stones
Type 1b stones look similar but have a teardrop or oval shape. They still show the same dark brown color and surface budding.
The difference in shape tells a deeper story. Type 1b stones form when your body transitions from favoring calcium oxalate dihydrate stones to favoring monohydrate stones. This shift often means you’re dealing with both hypercalciuria and hyperoxaluria at the same time.
Poor hydration and continued oxalate intake are major drivers behind the formation of this subtype.
🛒 Check Price & Purchase Stone Relief Pass AM/PM Bundle on Amazon
Type 1c Calcium Oxalate Monohydrate Stones
Type 1c stones are extremely rare and are tied to primary hyperoxaluria, a genetic disorder. These stones appear pale yellow or completely clear instead of dark brown.
Primary hyperoxaluria causes the body to produce high levels of oxalate on its own, overwhelming the kidneys. If dietary changes aren’t solving your stone issues and your stones are pale or clear, talk to your doctor about testing for primary hyperoxaluria.
Type 1d Calcium Oxalate Monohydrate Stones
Type 1d stones stand out because they look like beige pea gravel. They are round and smooth, completely different from other calcium oxalate stones.
These stones form when urine sits stagnant for too long in the kidney. Malformative uropathy or severe dehydrationcan both cause this stasis. If you have this stone type, it’s a red flag that urine flow is severely impaired and needs to be corrected to prevent future stones.
🛒 Check Price & Purchase Stone Relief Pass AM/PM Bundle on Amazon
Type 1e Calcium Oxalate Monohydrate Stones
Type 1e stones are rare but important to recognize. They are oval-shaped with very heavy surface budding, almost like a cauliflower.
These stones are linked to digestive disorders that impair how your body handles oxalate. Conditions like IBD, Crohn’s disease, chronic pancreatitis, or Type 2 diabetes can drive their formation. If you have one of these conditions and are still consuming oxalate, your risk skyrockets.
Cutting oxalate completely and healing your gut can prevent this stone type from coming back.

Final Thoughts on Calcium Oxalate Monohydrate Kidney Stones
Understanding the subtype of your calcium oxalate monohydrate kidney stones is a game changer. Whether you’re dealing with diet-driven stones, genetic mutations, or digestive complications, knowing the root cause lets you finally fix the problem.
I spent years stuck in a cycle of misinformation and wasted time. You don’t have to go through the same thing. By understanding your stone subtype and making the right changes, you can take full control over your kidney health and your life.